During an in vitro fertilization (IVF) cycle, after the eggs are retrieved, they are fertilized in a lab, where they grow for up to 6 days.
Under the supervision of an embryologist, there is a range of growth milestones that good quality embryos are expected to reach, and decisions are made based on what milestones are achieved and when.
Here is a guide to what is happening in the IVF lab day-by-day and what you should know about each stage.
Day 0 in the IVF Lab – Egg Retrieval and Fertilization
The day of the egg retrieval procedure is considered Day 0. On this day, you will have your eggs removed by your doctor under anesthesia, and the embryologist will assist in fertilizing them.
Fertilization with your partner's (or donor) sperm is done using either standard insemination or intracytoplasmic sperm injection (ICSI).
- Standard insemination occurs when the eggs and sperm are placed together, and fertilization happens naturally.
- ICSI is a procedure where the embryologist injects a single sperm into each egg. (For more insight, read An Intro to Intracytoplasmic Sperm Injection (ICSI).)
You should know in advance which method of insemination is planned to be used and if there are criteria by which that plan can be changed.
If ICSI is the chosen method of fertilization, the embryologist will know at the time of injection how many eggs of the retrieved eggs are mature. Only the mature eggs will be injected with sperm because immature eggs are not in a stage of development to accept a sperm and fertilize less often.
If standard insemination is being used, the sperm is placed with all of the eggs, and we will only know how many were mature the next morning when we check for fertilization.
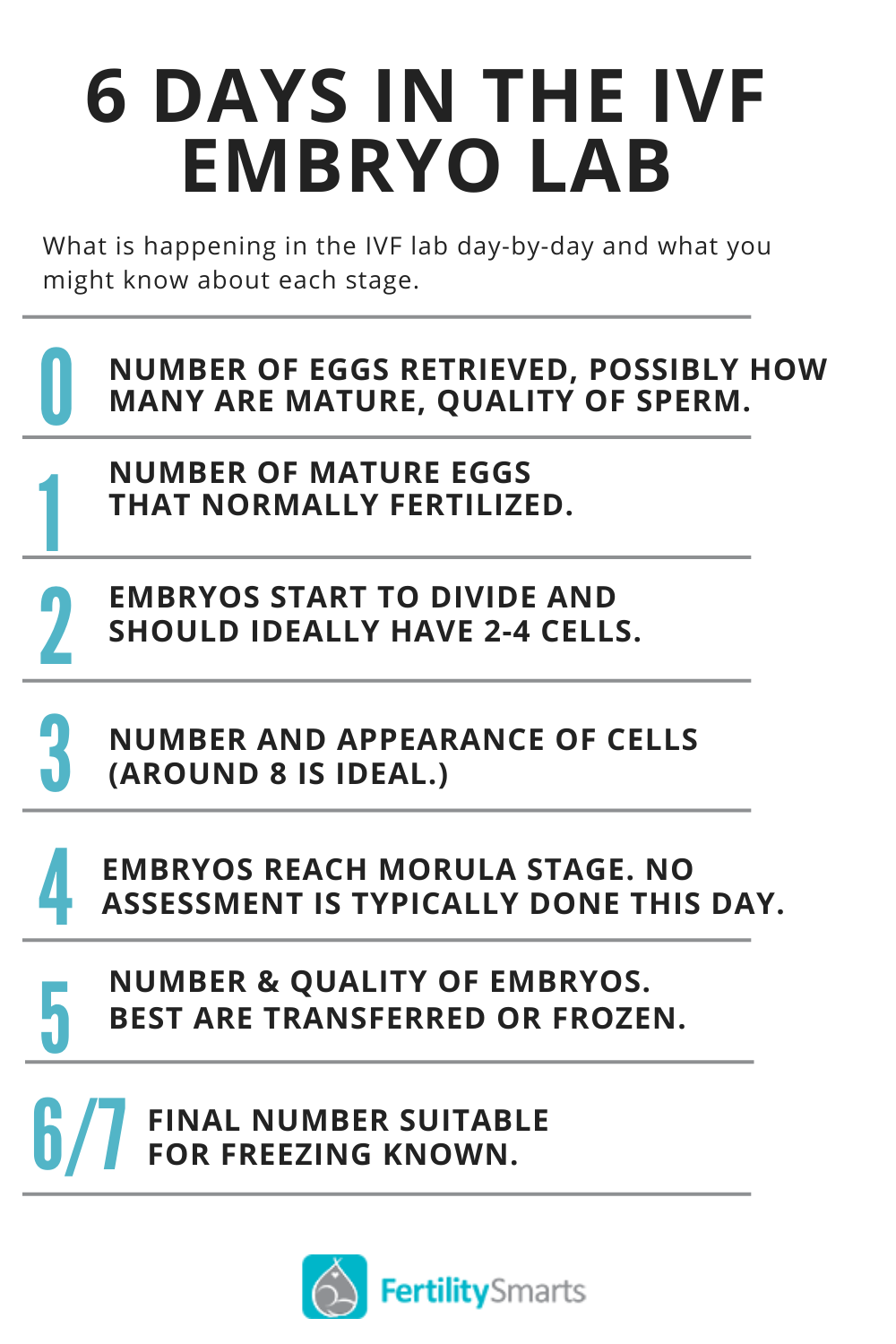
On Day 0, we know:
- The number of eggs that have been retrieved
- Possibly how many of the retrieved eggs are mature (If ICSI is performed)
- The quality of the sperm
For the most part, all eggs look the same at this stage, and they are not graded.
Day 1 in the IVF Lab – Number of Eggs Fertilized Known
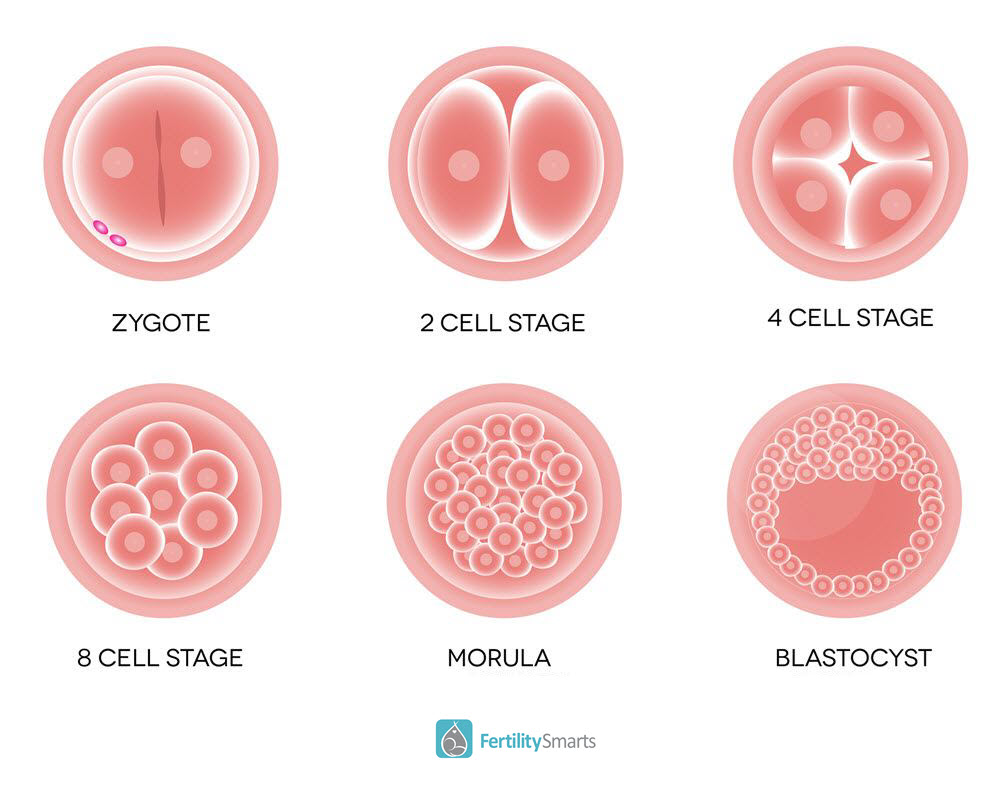
On Day 1, the eggs are checked for normal fertilization. The embryologists evaluate the eggs in the morning and can see which have normally fertilized by the presence of 2 round spheres in the middle of the egg called pronuclei. One of these pronuclei is the genetic material from the egg, and one is from the sperm.
All humans are a single cell for the first 24 hours of their life! Your embryologist or nurse will likely call you sometime during Day 1 to tell you the number of eggs that are normally fertilized.
On average,75% of the mature eggs will fertilize. Fertilized eggs are known as zygotes.
On Day 1, we know:
- The number of mature eggs normally fertilized.
- Day 1 embryos are not typically graded.
Day 2 in the IVF Lab – Embryo Divides
On Day 2, the embryos start to divide and should ideally have 2-4 cells. The embryo itself does not grow bigger; the single cell that was the fertilized egg hopefully divides to become 2 cells and then 4 cells, with each cell being half the size of its predecessor.
We can start to see slight variations between the embryos in the group, and they could be graded at this stage. Most clinics do not look at the embryos on this day, but it is possible to do an embryo transfer or freeze the embryos if that is the clinic's policy.
It is usually better to wait as long as possible for transfer and freezing as this allows more diversity within the group and enables the embryologist to more easily select the best embryos.
Day 3 in the IVF Lab – Embryo Grading and Potential Transfer
On Day 3, the embryos should be around 8 cells. This is the day we move them into a new Petri dish with different media (solution to support growth) similar to uterine fluid for their next stage of growth.
An average of 95% of fertilized eggs will grow to the Day 3 stage. Some clinics perform embryo transfers on Day 3, and some clinics wait until Day 5. Freezing can happen on any day of development up to Day 7. This depends on the number and quality of embryos that you have available and also the clinic policy.
We grade the embryos, but we still do not know how many will continue to grow to the blastocyst stage (Day 5 and 6).
On average, only half of all Day 3 embryos will continue to grow to the blastocyst stage, and the other half will stop growing after Day 3. Although embryologists do not know why embryos stop growing, it is thought it is because there is something wrong with their chromosomes.
If an embryo stops growing in the lab, it would most likely not have made a baby if we had transferred it.
On Day 3, we know:
- How many cells the embryos have
- If the embryos are of good appearance up to this point
- The appearance on Day 3 does not tell us how many embryos will continue to grow
Read: Embryo and Blastocyst Grading – How Does it Work?
Day 4 in the IVF Lab – From Cleavage Stage to Blastocyst
Day 4 is a transformation day where the embryos are in between the cleavage stage and blastocyst stage.
Many labs do not look at the embryos on this day, but if they did, we would see that some of them would be making the transition from a multi-celled embryo with clear cell outlines to what is called a morula which is the stage before an embryo becomes a blastocyst.
Sometimes embryos do not reach the morula stage until Day 5.
Day 5 in the IVF Lab – Blastocysts are Graded and Transferred or Frozen
On Day 5, embryos that have continued to grow to become blastocysts will have formed a fluid-filled cavity in the center of the embryo surrounded by a flat layer of cells called the trophectoderm (the part that makes the placenta).
These embryos should also have a clump of cells called the inner cell mass (the part that makes the baby).
Blastocyst embryos have a more complicated grading system based on 3 factors:
- The size of the embryo – based on the degree of expansion of the cavity (graded 2-6)
- The appearance of the inner cell mass cells (graded A-D)
- The appearance of the trophectoderm layer of cells (graded A-D)
Therefore an embryo with a grade of 4AA would be classed as a good quality embryo.
- Anything grade A is good quality.
- Anything with a B grade is classed as average.
- Anything C grade would be quite poor quality.
- Anything D grade would have cells that are not viable.
Why Embyo Grading?
Grading helps the embryologist to choose which embryo to transfer within your group of embryos. While the grading is a subjective evaluation, there are national standards, and the Center for Disease Control (CDC) requires all embryology labs to participate in proficiency testing for embryo grading.
Not all embryos grow at the same rate. Some will grow faster and be ready for transfer or freezing by Day 5, and some will need another day or two of growth to get to an advanced stage. This is a normal growth pattern.
Try not to over-analyze the exact grade of your embryos, as we have seen babies born from all grades of viable embryos.
On Day 5, we know:
- The number of embryos that have continued to grow and the quality of these embryos.
- The best embryos are either transferred or frozen on Day 5 according to your clinic's policy. In general, pregnancy rates are better when blastocyst stage embryos are transferred rather than Day 2-3 stage embryos.
Any embryos that are frozen are kept in the lab storage tanks until you need them. Any remaining slower-growing embryos are kept in the lab overnight, and there may or may not be more embryos to freeze on Day 6.
Read: 5 Things Your Embryologist Wants You To Know About Your IVF Procedure
Day 6 or 7 in the IVF lab – Final Number of Usable Embryos Known
On Day 6 or 7, we know the final number of embryos suitable for freezing. Day 6 or 7 is the final day in the lab for the embryos at most clinics.
The embryologists will assess the remaining embryos, and if they have continued to grow overnight, they will freeze all that are of good quality. Embryos that have not made a blastocyst by this day are not viable and will not be frozen.
Most labs do not grow embryos longer than Day 6 or 7 because they need to be frozen or in a uterus after Day 6 or 7.
Chromosome Screening
If you choose to undergo chromosome screening on your embryos, a single cell called a blastomere can be taken from each embryo on Day 3, or a small group of 3 to 5 cells can be taken at the blastocyst stage.
This is called embryo biopsy and is done before the embryos are frozen.
Chromosome screening allows us to select and thaw only genetically balanced embryos for transfer in a frozen embryo transfer cycle. This type of screening is recommended for women who:
- Have had multiple failed IVF cycles
- Have experienced recurrent pregnancy loss
- Who are of advanced maternal age (38 or older).
The pregnancy rates are very good for all ages of women when the embryos have been screened before transfer.
Hopefully, this has provided you with some insight as to what is happening in the lab when embryos are created, typical growth patterns that embryos undergo, and the kind of information you can expect to receive while undergoing this process.