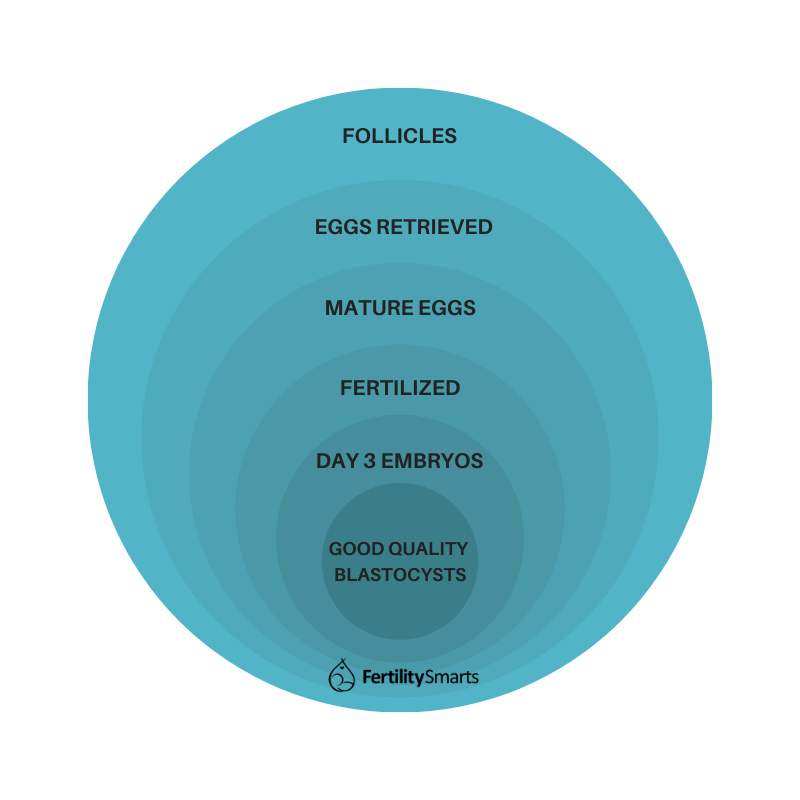
Undoubtedly, one of the biggest surprises with in vitro fertilization (IVF) is the dramatic drop or loss of eggs/embryos. Many people assume that if they have 10 eggs collected, that’s 10 embryos, which means 1 fresh transfer and 9 in the freezer.
Unfortunately, that can be far from true and there are multiple steps along the way that results can take an unexpected turn. This "numbers game" is what is known as IVF attrition. There are no set rules for this game, meaning that it's impossible for a doctor to predict what may happen with a patient. In addition, results can vary from person to person.
So what are realistic expectations? As an embryologist, I can share what is generally known about IVF attrition.
Attrition With Egg Retrieval
In an IVF cycle, medication is used to hyper-stimulate ovaries to develop multiple follicles that hopefully contain eggs. Constant monitoring with ultrasound is done and you should get an idea of how many eggs are expected to be collected based on the size of your follicles at the ultrasound and your estrogen levels. (Read more about preparing for your egg retrieval.)
Straight up, you may not get as many eggs collected as you expect:
- Some follicles stimulate that have nothing in them.
- Sometimes when the doctor goes in and looks around, some of the follicles just aren’t there anymore.
- Sometimes at egg collection when I assess the fluid I see large masses of cumulus cells (the support cells that surround an egg) that do not contain an egg inside. Even though there is no egg, it may lead to a growing follicle and be an expected egg.
So, please note: the number of follicles seen on ultrasound does not necessarily equal the number of eggs that will be retrieved. Attrition in the IVF process happens right from the start.
That said, I’ve also seen a patient devastated to end up with only 1 egg go on to have a baby from that single egg.
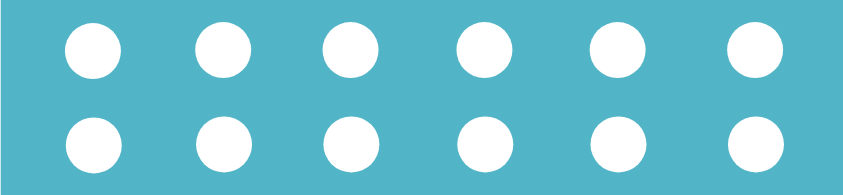
Example: Let's use a hypothetical scenario where there are 12 eggs retrieved.
Attrition During Fertilization
After the egg collection, approximately 4-6 hours later, the eggs get inseminated with sperm. This can happen with either:
Your specialist will make the decision of which one is best for your situation.
Mature Eggs Only
Not all eggs that are retrieved are able to be fertilized. Eggs start off with 46 chromosomes and need to undergo a process of shedding extra chromosomes to become a mature egg. For fertilization to properly occur, a healthy egg cell should have 23 chromosomes that can pair with the 23 chromosomes from a sperm cell.
If ICSI is being performed, only the mature eggs can be injected and it’s common to have some eggs that are not. So, straight up, there is a loss in numbers here.
Overall, it’s expected that about 80% of eggs should be mature, but just as with every step I’m going to discuss, this can vary greatly among patients—and even one person's subsequent cycles.
Example: We will assume 10 out of 12 eggs or 80% are mature.
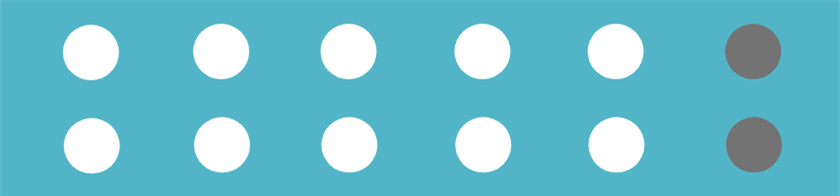
I commonly see many patients have all mature eggs, but it’s very common to see some immature ones in there as well. Very rarely, they can all be immature!
If IVF is being done, all eggs are going to get inseminated (as eggs are left in their fluffy cumulus cells) and the next morning we will see which ones are fertilized. Again, the immature ones will not fertilize.
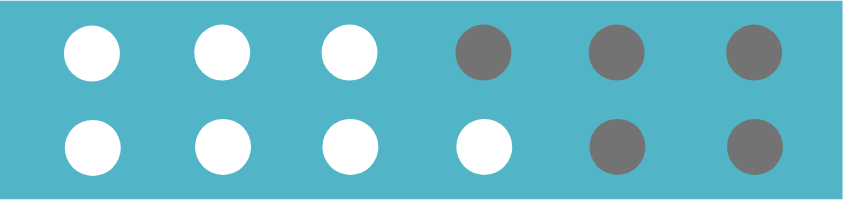
Fertilization Rates
With 12 eggs collected, 10 can be injected with ICSI, or only 10 will be able to be fertilized by the sperm with IVF. Of those mature eggs that are capable of fertilizing, they are not all expected to fertilize. Approximately 70-80% is a good fertilization rate but many labs are happy with less than this as they may treat poorer prognosis patients that aren’t expected to do as well.
Absolutely, I see many patients get 100% fertilization, but it’s important to know that seeing some not fertilize is completely normal. We may also see some that fertilize abnormally and need to be discarded.
I’ve also seen people who had only a small fraction of their eggs fertilize get pregnant from the few embryos they had.
Fertilization results can be a common point of disappointment among patients.
Example: Let's assume that 7 out of 10 eggs or 70% fertilize properly.
Attrition During Embryo to Blastocyst Development
Most fertilized eggs, or embryos as they now are, will divide onto a day 3 embryo; as the cells divide, the quality may start to deteriorate, cell fragment, and may divide unevenly (read more about embryo grading). For this reason, not all embryos will be suitable for transfer or freeze on day 3 if your doctor/clinic has chosen day 3 for you.
While this may be disappointing, please know that it’s this process that allows us to choose the ones that are best for use and allows some genetically abnormal embryos to deselect themselves from the batch. These embryos would not have been capable of forming a healthy pregnancy.
This process allows us to choose the ones that are best for use and allows some genetically abnormal embryos to deselect themselves from the batch.
The Day 3 Drop
A big drop in numbers usually occurs in the phase between day 3 and day 5 of embryo development. We fully expect that not all embryos will be able to form a blastocyst and this is because the egg has everything in it to drive growth to get to day 3 and then embryonic genome activation (EGA) has to occur.
This means that embryo development is under the control of the maternal egg genes until day 3 and then control is taken over by the genes of the zygote which many embryos just can’t do and commonly is because of a chromosomal problem. It’s an advantage to grow to day 5 as only the developmentally competent embryos are able to reach blastocyst.
It’s an advantage to grow to day 5 as only the developmentally competent embryos are able to reach blastocyst.
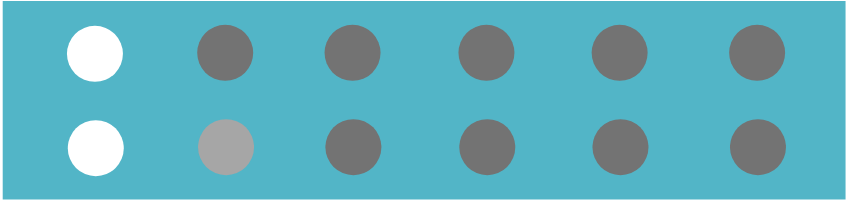
A day 3 embryo is a little bundle of 6-10 cells and there are major growth and structural changes that need to happen to reach the stage of a 100-150 cell blastocyst, so the poorer quality embryos may arrest, or stop developing at this stage.
It is also possible that embryos make it to blastocyst but are just too poor quality to warrant a transfer or freeze. A lot of patients do not realize that this is a possibility.
Blastocyst Success Rates
You may see it written that 30-50% of day 3 embryos might be expected to reach blastocyst. Keep in mind that this is going to differ from person to person and is very hard to provide specific stats on due to the many variations and factors at play from age of the egg used to the genetics in each sex cell and how they combine.
It's not just numbers but the quality that is important too. I’ve seen patients with over 12 eggs and very good fertilization not have anything suitable for transfer or freeze due to poor quality.
Example: Using the general estimate of 30-50%, we would expect 2 or 3 blastocysts to remain for a fresh or frozen transfer.
While much of this information can be stressful, please know this is a basic guideline. Many patients do much better than this, although, it is also true that some will not do as well.
Receiving Unexpected Results
If you have been faced with any of these unexpected results, please know that this situation has been faced by many people before you and you are not alone. Having a poor cycle doesn’t necessarily mean you will get the same results again. There are different medical protocols or lab options (such as different day embryo transfer, fresh/frozen, IVF/ICSI) that may lead to you getting different results in a subsequent cycle.
Having a poor cycle doesn’t necessarily mean you will get the same results again
From my experience, it's common to be shocked at how an IVF cycle plays out, so please know, it is normal to see a continual drop in numbers and is what hopefully leads us to the few best embryos that will give you your baby.